Maureen Hennessey, Ph.D. | SVP, Director, Value Transformation
Christopher Terrone | VP, Healthcare Insights, Market Access
May is Mental Health Awareness Month, a time to reaffirm our commitment to supporting individuals living with behavioral health conditions. At Precision AQ, we believe everyone deserves access to the care and medications needed to optimize their health and quality of life.
One of the most impactful ways we can advance that commitment is by improving access to evidence-based treatments for serious mental health conditions. Schizophrenia and bipolar disorder are two such conditions: chronic and often profoundly disruptive without consistent care. For many individuals, long-acting medications (LAMs) offer a critical lifeline, reducing the risks of neurodegeneration and relapse, supporting medication adherence, and improving long-term outcomes.
This spring, the National Council for Mental Wellbeing released a Guide to Long-Acting Medications, highlighting the clinical value of LAMs and calling on organizations to expand their use. In response, Precision AQ conducted a survey of health system decision makers with knowledge of their organization’s use of antipsychotic LAMs for individuals living with schizophrenia and bipolar conditions, to better understand current practices, barriers, and opportunities.
Challenging the Legacy Mindset
A key insight from our survey: a persistent legacy mindset continues to delay optimal treatment. Many organizations still reserve LAMs for patients who have already failed oral therapies. This approach may limit access to effective treatment and undermines patient outcomes.
Barriers and Drivers to LAM Use
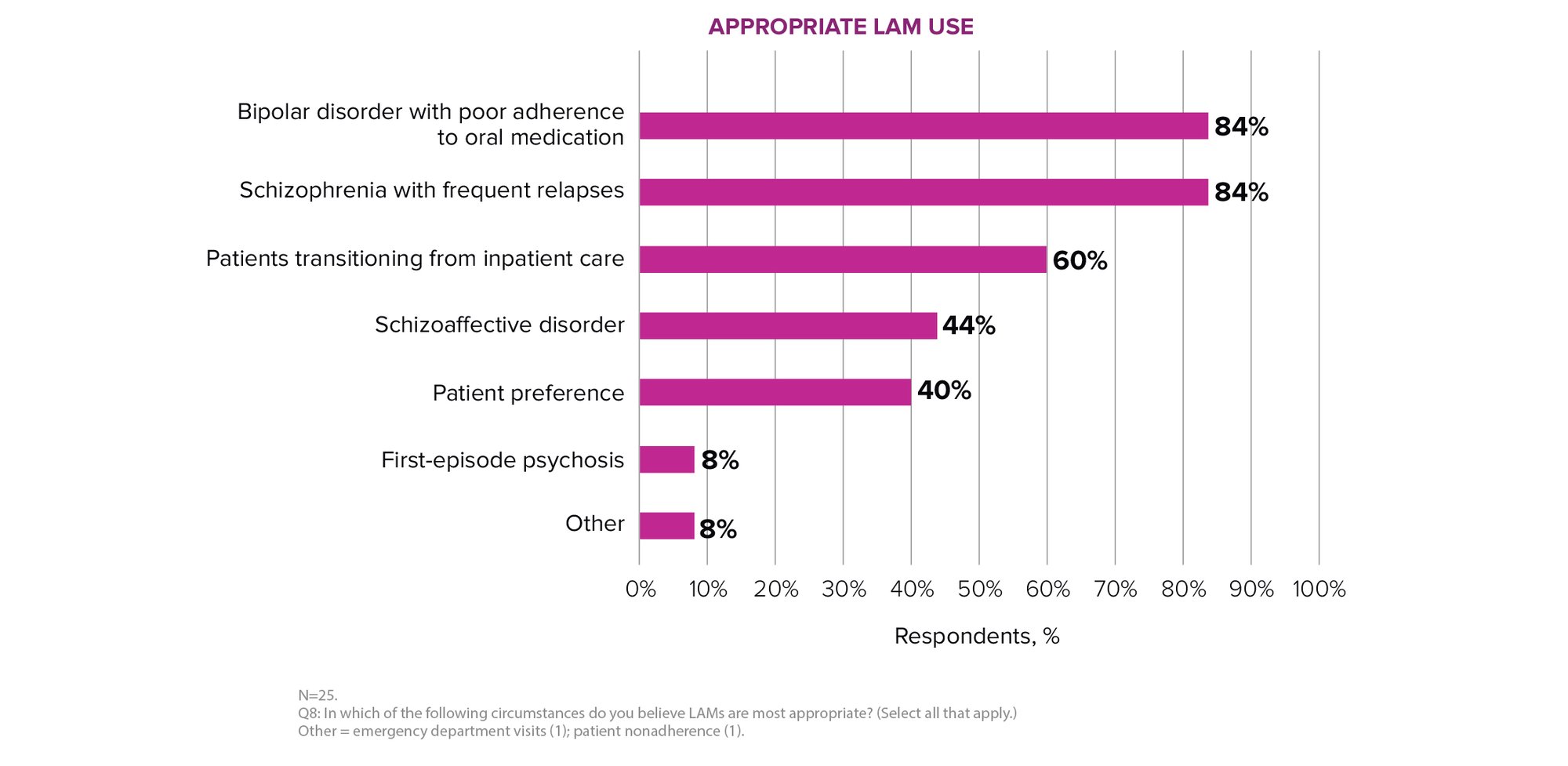
Use Cases Reflecting the Legacy Mindset: LAMs are most commonly used for persons with bipolar disorder with poor oral adherence (84%) and schizophrenia with frequent relapse (84%). Only 8% reported using LAMs for individuals experiencing first-episode psychosis—a potential missed opportunity for early intervention.
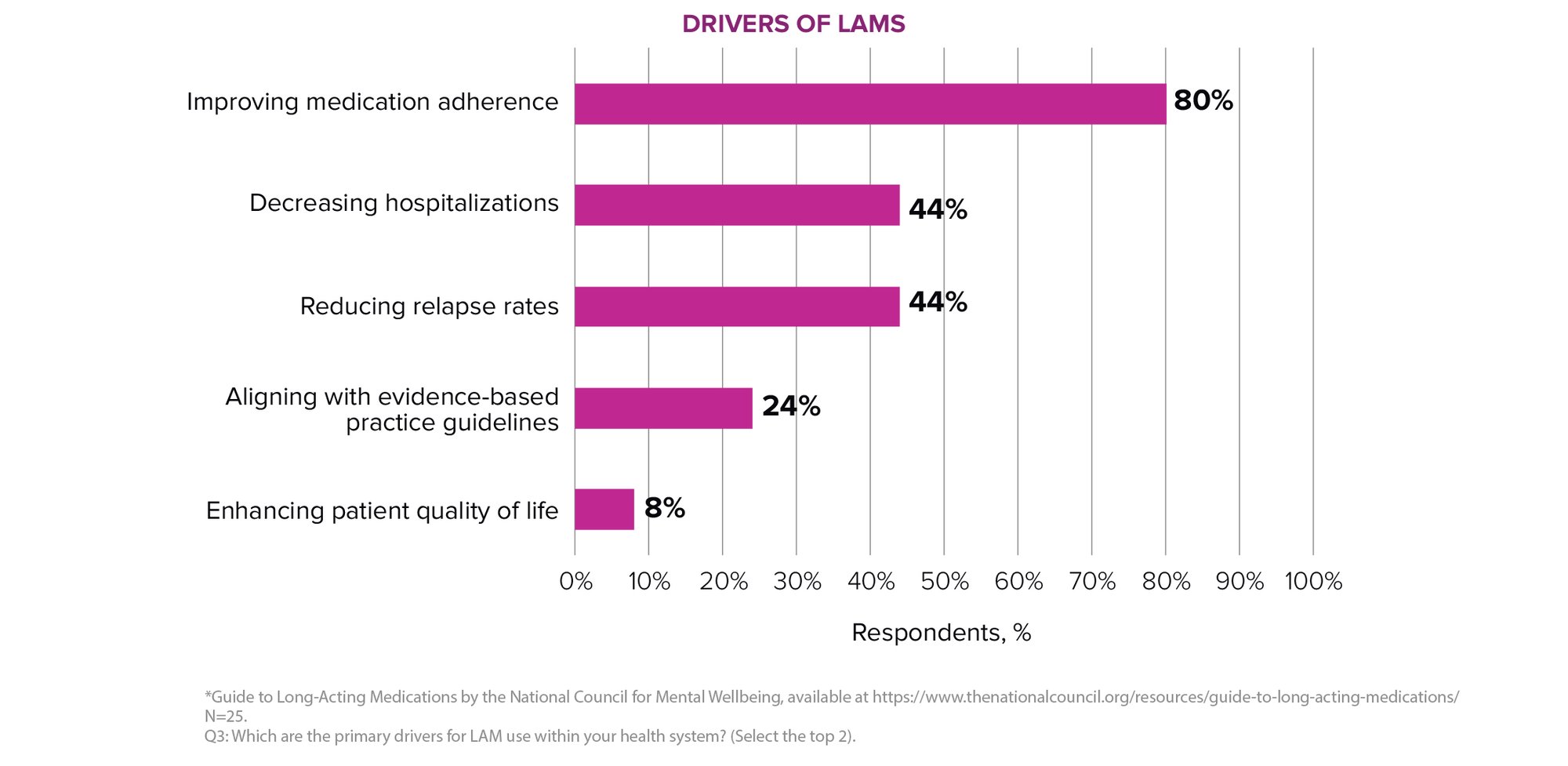
Drivers of Use: The most cited drivers of LAM use were to improve medication adherence (80%), followed by reducing relapse rates and hospitalizations. However, this reflects a reactive approach where LAMs are introduced only after problems arise. The Guide to Long-Acting Medications advocates for a proactive strategy, especially in early-stage illness.
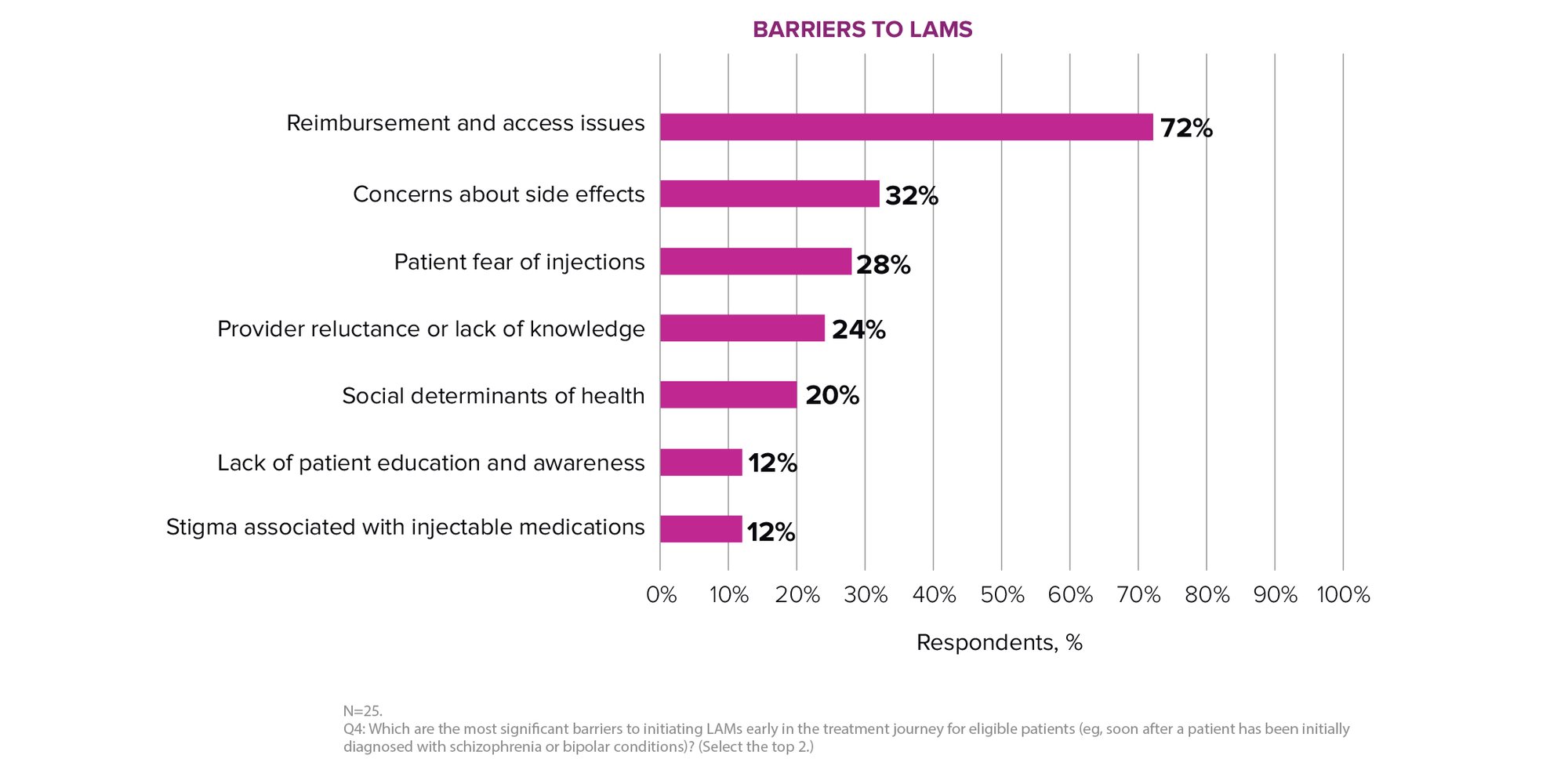
Barriers to Early Use: Reimbursement and access issues (72%), including prior authorizations and formulary restrictions, were selected as the top barriers. These requirements often force patients to demonstrate non-adherence to oral medications before qualifying for LAMs, reinforcing the legacy mindset.
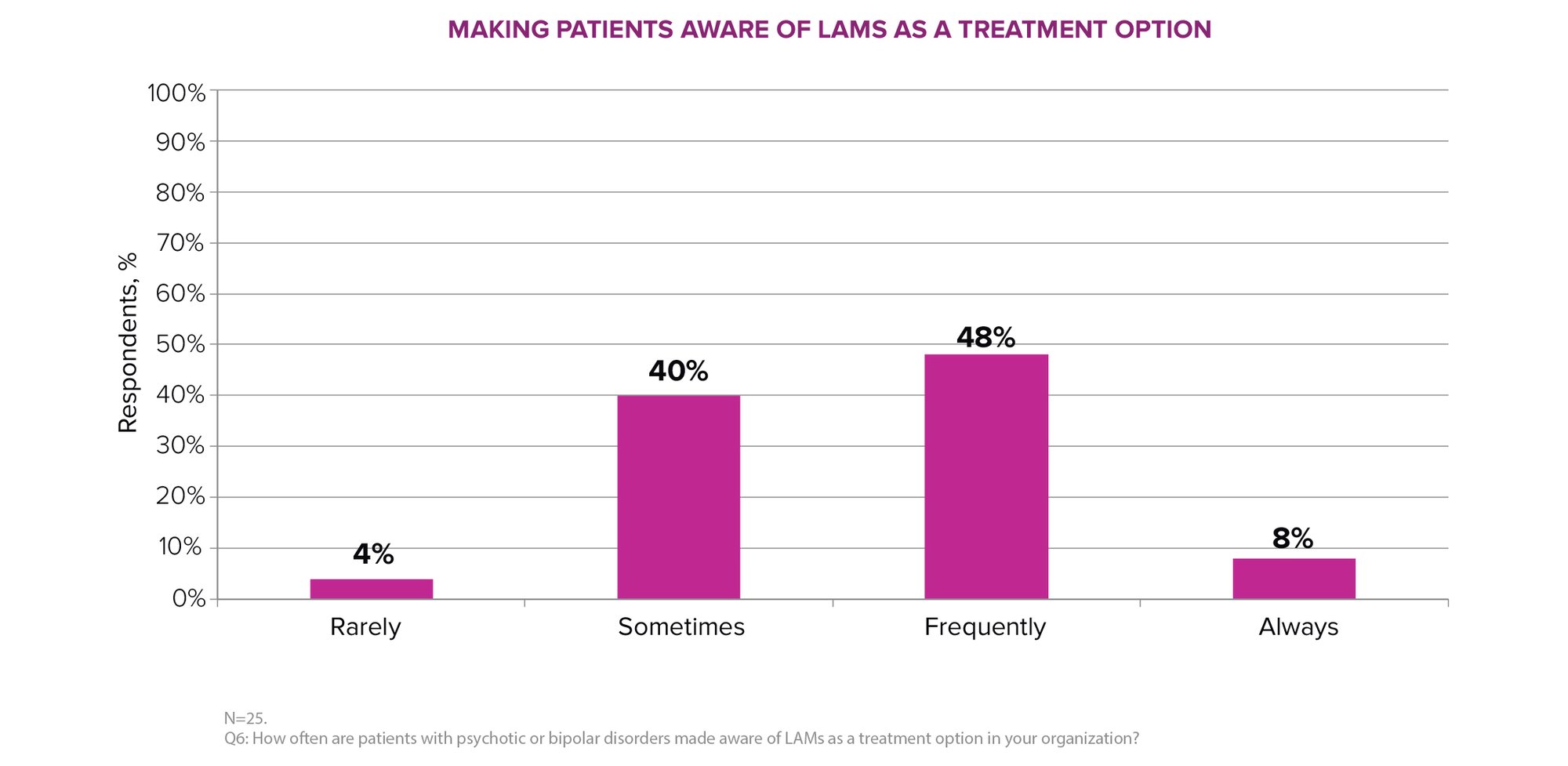
Inconsistent Patient Awareness: Only 8% of respondents said patients are “always” informed about LAMs as a treatment option. This highlights the need for standardized education and shared decision-making protocols.
Steps to advance access
To shift away from the legacy mindset that limits early use of long-acting medications (LAMs), we must take deliberate steps to modernize clinical practice, streamline access, and empower both providers and patients. The following actions can help drive that transformation:
- Promote Early Use: Encourage providers to consider LAMs earlier in the treatment journey by integrating shared decision-making and CQI (Continuous Quality Improvement) practices.
- Streamline Access: Collaborate with payers to revise prior authorization criteria and reduce access barriers for patients newly diagnosed with schizophrenia or bipolar disorder.
- Enhance Education: Equip providers and patients with clear, accessible educational materials to raise awareness and understanding of LAMs as a treatment option.
- Expand Support Programs: Offer financial assistance and logistical support (e.g., in-home administration, transportation) to improve patient access and adherence.
For more information about our survey or to speak with one of our experts, contact us.
